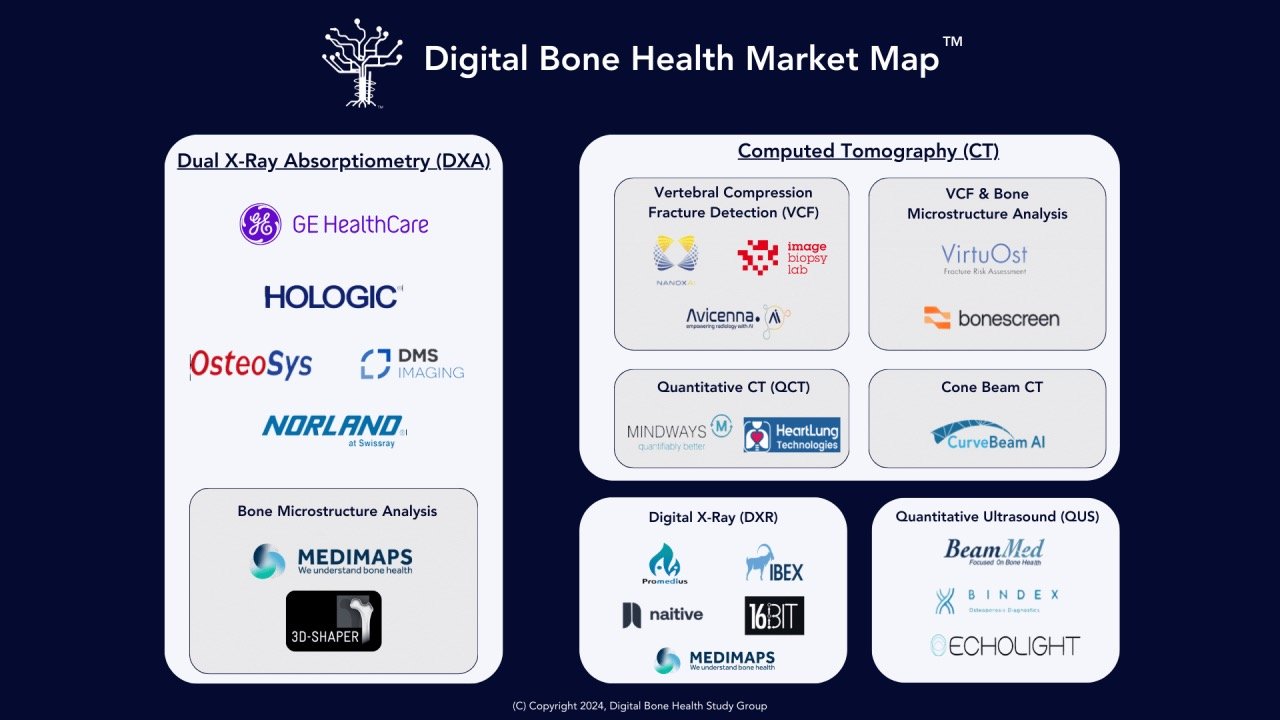
Digital Bone Health - An Emerging Market Sector
I created this Map to begin outlining the emerging commercial efforts to address the global epidemic of low bone mass and fragility fractures through algorithmic diagnostic imaging analysis and reporting technologies. These efforts mainly aim to detect and confirm undiagnosed patients with low bone mass and flag them for preventive intervention of either primary or secondary fractures.
Emerging Digital Bone Health Market - Part II
Integrating AI into fracture risk assessment within existing clinical workflows has the potential to revolutionize the management of osteoporosis by enabling opportunistic detection at the point of care. Despite the advancements in AI technologies for X-ray and CT scans now available in the US, the fee-for-service model and reimbursement challenges present significant barriers to their widespread adoption. Despite the proven capability of being integrated non-disruptively into existing clinical work flows in markets outside the US, there currently is little incentive in US healthcare to prioritize adoption of these technologies where they could have the most effect.
Will 2025 Be a Breakout Year for Digital Bone Health?
In recent years, advances in digital health technologies are transforming the landscape of musculoskeletal care. From imaging innovations to AI-powered diagnostics, the field of bone health has seen steady, yet slower advancements. However, with increasing awareness of osteoporosis and fracture prevention, and emerging digital tools to manage this condition, 2025 could mark a turning point towards conditions for wider adoption and impact in digital bone health.
The Coming Disruption of Fracture Liaison Services in the Era of AI-Driven Imaging Detection Tools
The landscape of bone health management is ripe for a seismic shift with the advent of AI-driven imaging technologies. These tools are set to revolutionize osteoporosis diagnosis and fracture risk assessment, fundamentally altering how patients are identified and treated. However, the current Fracture Liaison Service (FLS) model, operating within a fee-for-service healthcare environment, is neither scalable nor sustainable in the face of this impending transformation.

